Getting The Dementia Fall Risk To Work
Table of ContentsNot known Facts About Dementia Fall RiskThe Only Guide for Dementia Fall RiskAll About Dementia Fall RiskIndicators on Dementia Fall Risk You Should Know
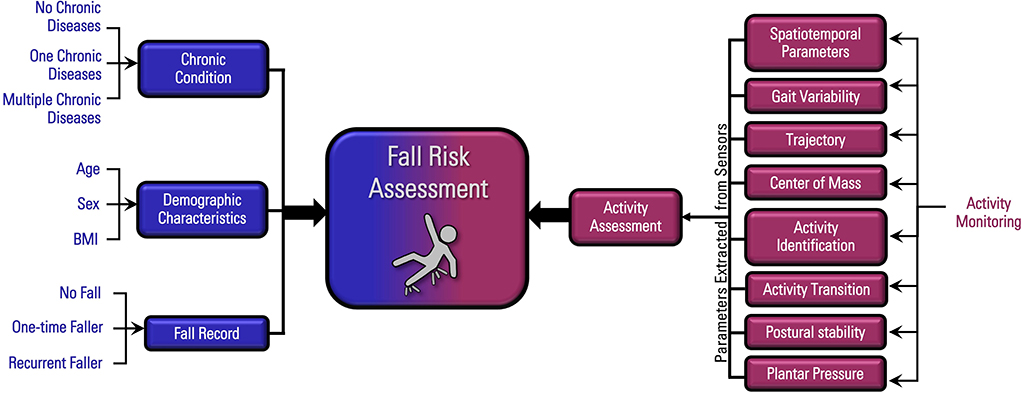
A fall risk assessment checks to see how most likely it is that you will certainly drop. It is mainly done for older adults. The analysis generally consists of: This includes a collection of inquiries regarding your general health and if you've had previous drops or issues with balance, standing, and/or walking. These devices check your stamina, balance, and stride (the method you walk).STEADI includes testing, examining, and intervention. Treatments are suggestions that may lower your danger of dropping. STEADI includes 3 steps: you for your threat of falling for your risk aspects that can be improved to attempt to stop falls (as an example, balance issues, impaired vision) to minimize your risk of dropping by utilizing effective techniques (for example, supplying education and learning and sources), you may be asked several concerns consisting of: Have you fallen in the previous year? Do you really feel unsteady when standing or strolling? Are you fretted about dropping?, your provider will check your strength, balance, and stride, using the complying with loss assessment devices: This examination checks your gait.
Then you'll take a seat once more. Your service provider will certainly examine for how long it takes you to do this. If it takes you 12 seconds or more, it might imply you go to greater risk for an autumn. This test checks toughness and equilibrium. You'll rest in a chair with your arms crossed over your chest.
The settings will certainly get more difficult as you go. Stand with your feet side-by-side. Move one foot midway forward, so the instep is touching the huge toe of your various other foot. Relocate one foot fully in front of the other, so the toes are touching the heel of your various other foot.
What Does Dementia Fall Risk Do?
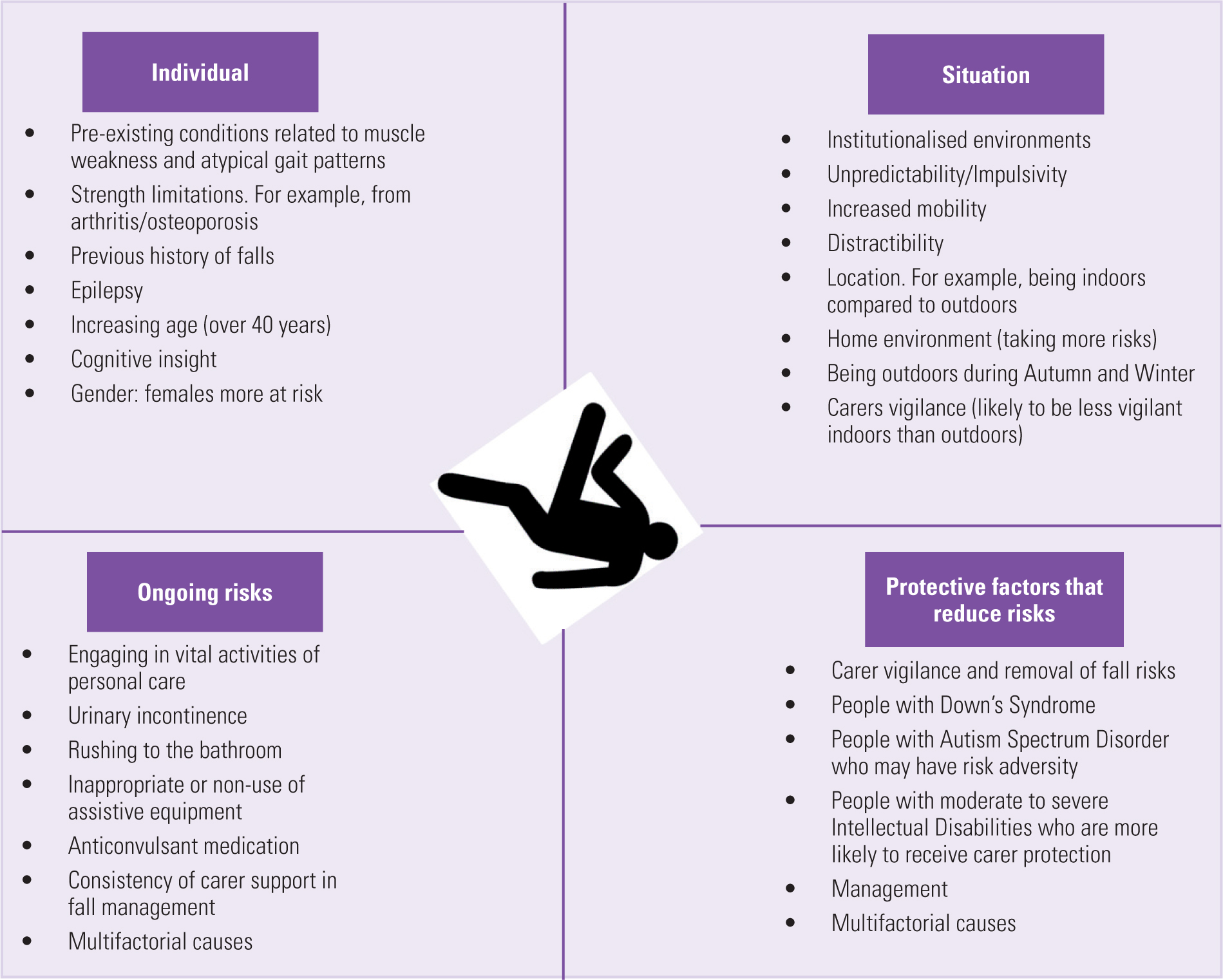
Many falls occur as an outcome of multiple adding factors; for that reason, taking care of the threat of dropping begins with recognizing the aspects that add to fall risk - Dementia Fall Risk. A few of the most pertinent threat factors consist of: History of prior fallsChronic clinical conditionsAcute illnessImpaired stride and balance, lower extremity weaknessCognitive impairmentChanges in visionCertain risky medicines and polypharmacyEnvironmental factors can additionally increase the threat for drops, including: Inadequate lightingUneven or harmed flooringWet or unsafe floorsMissing or harmed handrails and order barsDamaged or incorrectly equipped devices, such as beds, wheelchairs, or walkersImproper use assistive devicesInadequate guidance of the people living in the NF, consisting of those that exhibit hostile behaviorsA effective autumn threat administration program needs a detailed professional analysis, with input from all participants of the interdisciplinary team

The care plan must likewise consist of treatments that are system-based, such as those that promote a risk-free atmosphere (ideal lights, handrails, grab bars, and so on). The more tips here effectiveness of the interventions ought to be assessed regularly, and the care plan modified as needed to mirror adjustments in the fall risk assessment. Implementing a fall risk management system making use of evidence-based ideal technique can minimize the occurrence of falls in the NF, while limiting the possibility for fall-related injuries.
The Definitive Guide for Dementia Fall Risk
The AGS/BGS guideline advises screening all grownups aged 65 years and older for loss danger annually. This testing consists of asking people whether they have dropped 2 or more times in the previous year or sought medical attention for an autumn, or, if they have not fallen, whether they feel unsteady when strolling.
People that have dropped once without injury must have their balance and stride evaluated; those with gait or equilibrium irregularities should get added my response evaluation. A history of 1 autumn without injury and without stride or equilibrium issues does not necessitate additional analysis beyond continued yearly fall danger testing. Dementia Fall Risk. A fall danger analysis is required as part of the Welcome to Medicare assessment
More About Dementia Fall Risk
Recording a falls background is one of the quality indications for loss avoidance and administration. A crucial component of danger assessment is a medicine evaluation. A number of classes of medications raise autumn risk (Table 2). copyright medications particularly are independent predictors of drops. These drugs often tend to be sedating, change the sensorium, and harm equilibrium and stride.
Postural hypotension can usually be reduced by lowering the dose of blood pressurelowering drugs and/or stopping medicines that have orthostatic hypotension as a negative effects. Use above-the-knee assistance tube and copulating the head of the bed elevated might also reduce postural reductions in blood pressure. The preferred components of a fall-focused physical exam are displayed in Box 1.
A TUG read here time higher than or equivalent to 12 secs recommends high loss threat. Being incapable to stand up from a chair of knee height without utilizing one's arms suggests boosted loss threat.